
I believe I just took a courageous first step toward reality and maturity
I think it resulted from having experienced a moment of clarity, today.
After months of hearing about hospice from my reading, research, conventions, spiritual friends, and hospice volunteers, I have moved forward in coming to terms with endings and with the fact that our family needs help dealing with all this emotionally. My dad is an angry wreck and I want to cry because of emotions I don't know how to handle.
On several occasions, in 2005, Dr. Thomas of the Little Company of Mary Hospital in Chicago informed me my Mom would not live long and needed hospice care. I summarily dismissed his comments, brought my mom home to be alongside her husband in her home, and proceeded to hire round-the-clock care to care for her in the convert of home. One of the nurses assigned to us after my mom's nursing home stay, completed a form and checked off the box indicating that my mom had less than six months to live.
There has been much evidence of an ending; I have ignored it.
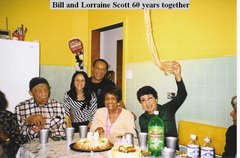
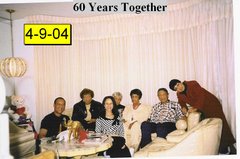
As a result of my mom's being with her husband of 63 years, in her house she loves, well taken care of by round-the-clock caregivers, and receiving regular visitors from friends, she is doing okay. She has beaten all the odds.
When I attended my second caregiver conference last week, I learned a whole new definition of hospice. I always believed hospice was a place where terminally ill people go to die within days or weeks.
I learned that hospice is more than just a place. It is a service. A service that provides palliative care and help with bereavement.
According to VITAS, the nation's largest hospice provider, End-of-life patient care pushes and tests us every day. Each day is a new life for hospice patients, continually creating new demands on caregivers. Each day, hospice must re-define itself to address the dynamic needs of patients and families.
Caring Connections, a program of the National Hospice and Palliative Care Organization (NHPCO), is a national consumer engagement initiative to improve care at the end of life, supported by a grant from The Robert Wood Johnson Foundation. They provide the following descriptions of hospice services from their website: caringinfo.org
How Does Hospice Work?
Hospice care is for any person who has a life-threatening or terminal illness. Most reimbursement sources require a prognosis of six months or less if the illness runs its normal course. Patients with both cancer and non-cancer illnesses are eligible to receive hospice care. All hospices consider the patient and family together as the unit of care.
The majority of hospice patients are cared for in their own homes or the homes of a loved one. “Home” may also be broadly construed to include services provided in nursing homes, hospitals and prisons.
Typically, a family member serves as the primary caregiver and, when appropriate, helps make decisions for the terminally ill individual. Members of the hospice staff make regular visits to assess the patient and provide additional care or other services. Hospice staff is on-call 24 hours a day, seven days a week.
Who is the Hospice Team?
Hospice care is a family-centered approach that includes, at a minimum, a team of doctors, nurses, social workers, counselors, and trained volunteers. They work together focusing on the dying patient’s needs; physical, psychological, or spiritual. The goal is to help keep the patient as pain-free as possible, with loved ones nearby until death. The hospice team develops a care plan that meets each patient's individual needs for pain management and symptom control.
· It is important to find out what the role of the patient's primary doctor will be once the patient begins receiving hospice care. Most often, hospice patients can choose to have their personal doctor involved in the medical care. Both the patient's physician and the hospice medical director may work together to coordinate the patient's medical care, especially when symptoms are difficult to manage. Regardless, a physician's involvement is important to ensure quality hospice care. The hospice medical director is also available to answer questions you or the patient may have regarding hospice medical care.
The team usually consists of:
The patient' s personal physician;
Hospice physician (or medical director);
Nurses;
Home health aides;
Social workers;
Clergy or other counselors;
Trained volunteers; and
Speech, physical, and occupational therapists, if needed.
What Services Does the Hospice Team Provide?
Among its major responsibilities, the interdisciplinary hospice team:
Manages the patient’s pain and symptoms;
Assists the patient with the emotional and psychosocial and spiritual aspects of dying;
Provides needed medications, medical supplies, and equipment;
Coaches the family on how to care for the patient;
Delivers special services like speech and physical therapy when needed;
Makes short-term inpatient care available when pain or symptoms become too difficult to manage at home, or the caregiver needs respite time; and
Provides bereavement care and counseling to surviving family and friends.
In many cases, family members or loved ones are the patient's primary care givers. Additionally, hospice recognizes that loved ones have their own special needs for support. As a relationship with the hospice begins, hospice staff will want to know about the primary caregiver's priorities. They will also want to know how best to support the patient and family during this time. Support can take many different forms, including visits with the patient and family members; telephone calls to loved ones, including family members who live at a distance, about the patient’s condition; and the provision of volunteers to assist with patient and family needs.
Counseling services for the patient and loved ones are an important part of hospice care. After the patient's death, bereavement support is offered to families for at least one year. These services can take a variety of forms, including telephone calls, visits, written materials about grieving, and support groups. Individual counseling may be offered by the hospice or the hospice may make a referral to a community resource.
I decided to go online to locate VITAS closest to my parents and picked up that heavy telephone to determine how the Scott family can receive their services.
I spoke with Cindy a helpful call center specialist. I provided her with my mother’s and father’s Social Security numbers, insurance information and medical diagnoses. She says the next steps are to have their doctor contact them to authorize hospice service. Once they receive that call, they will send out a registered admissions nurse to conduct an assessment of why parents need.
Hopefully, they will be able to schedule an appointment with the registered admissions nurse to coincide with my upcoming trip to Chicago at the end of the week: May 31 through June 5, 2007.
I will keep my fingers crossed, that my parents will both be accepted and that we will soon begin to receive professional help with things we don't know how to handle emotionally.
I will keep you posted on the outcome.
I think it resulted from having experienced a moment of clarity, today.
After months of hearing about hospice from my reading, research, conventions, spiritual friends, and hospice volunteers, I have moved forward in coming to terms with endings and with the fact that our family needs help dealing with all this emotionally. My dad is an angry wreck and I want to cry because of emotions I don't know how to handle.
On several occasions, in 2005, Dr. Thomas of the Little Company of Mary Hospital in Chicago informed me my Mom would not live long and needed hospice care. I summarily dismissed his comments, brought my mom home to be alongside her husband in her home, and proceeded to hire round-the-clock care to care for her in the convert of home. One of the nurses assigned to us after my mom's nursing home stay, completed a form and checked off the box indicating that my mom had less than six months to live.
There has been much evidence of an ending; I have ignored it.
As a result of my mom's being with her husband of 63 years, in her house she loves, well taken care of by round-the-clock caregivers, and receiving regular visitors from friends, she is doing okay. She has beaten all the odds.
When I attended my second caregiver conference last week, I learned a whole new definition of hospice. I always believed hospice was a place where terminally ill people go to die within days or weeks.
I learned that hospice is more than just a place. It is a service. A service that provides palliative care and help with bereavement.
According to VITAS, the nation's largest hospice provider, End-of-life patient care pushes and tests us every day. Each day is a new life for hospice patients, continually creating new demands on caregivers. Each day, hospice must re-define itself to address the dynamic needs of patients and families.
Caring Connections, a program of the National Hospice and Palliative Care Organization (NHPCO), is a national consumer engagement initiative to improve care at the end of life, supported by a grant from The Robert Wood Johnson Foundation. They provide the following descriptions of hospice services from their website: caringinfo.org
How Does Hospice Work?
Hospice care is for any person who has a life-threatening or terminal illness. Most reimbursement sources require a prognosis of six months or less if the illness runs its normal course. Patients with both cancer and non-cancer illnesses are eligible to receive hospice care. All hospices consider the patient and family together as the unit of care.
The majority of hospice patients are cared for in their own homes or the homes of a loved one. “Home” may also be broadly construed to include services provided in nursing homes, hospitals and prisons.
Typically, a family member serves as the primary caregiver and, when appropriate, helps make decisions for the terminally ill individual. Members of the hospice staff make regular visits to assess the patient and provide additional care or other services. Hospice staff is on-call 24 hours a day, seven days a week.
Who is the Hospice Team?
Hospice care is a family-centered approach that includes, at a minimum, a team of doctors, nurses, social workers, counselors, and trained volunteers. They work together focusing on the dying patient’s needs; physical, psychological, or spiritual. The goal is to help keep the patient as pain-free as possible, with loved ones nearby until death. The hospice team develops a care plan that meets each patient's individual needs for pain management and symptom control.
· It is important to find out what the role of the patient's primary doctor will be once the patient begins receiving hospice care. Most often, hospice patients can choose to have their personal doctor involved in the medical care. Both the patient's physician and the hospice medical director may work together to coordinate the patient's medical care, especially when symptoms are difficult to manage. Regardless, a physician's involvement is important to ensure quality hospice care. The hospice medical director is also available to answer questions you or the patient may have regarding hospice medical care.
The team usually consists of:
The patient' s personal physician;
Hospice physician (or medical director);
Nurses;
Home health aides;
Social workers;
Clergy or other counselors;
Trained volunteers; and
Speech, physical, and occupational therapists, if needed.
What Services Does the Hospice Team Provide?
Among its major responsibilities, the interdisciplinary hospice team:
Manages the patient’s pain and symptoms;
Assists the patient with the emotional and psychosocial and spiritual aspects of dying;
Provides needed medications, medical supplies, and equipment;
Coaches the family on how to care for the patient;
Delivers special services like speech and physical therapy when needed;
Makes short-term inpatient care available when pain or symptoms become too difficult to manage at home, or the caregiver needs respite time; and
Provides bereavement care and counseling to surviving family and friends.
In many cases, family members or loved ones are the patient's primary care givers. Additionally, hospice recognizes that loved ones have their own special needs for support. As a relationship with the hospice begins, hospice staff will want to know about the primary caregiver's priorities. They will also want to know how best to support the patient and family during this time. Support can take many different forms, including visits with the patient and family members; telephone calls to loved ones, including family members who live at a distance, about the patient’s condition; and the provision of volunteers to assist with patient and family needs.
Counseling services for the patient and loved ones are an important part of hospice care. After the patient's death, bereavement support is offered to families for at least one year. These services can take a variety of forms, including telephone calls, visits, written materials about grieving, and support groups. Individual counseling may be offered by the hospice or the hospice may make a referral to a community resource.
I decided to go online to locate VITAS closest to my parents and picked up that heavy telephone to determine how the Scott family can receive their services.
I spoke with Cindy a helpful call center specialist. I provided her with my mother’s and father’s Social Security numbers, insurance information and medical diagnoses. She says the next steps are to have their doctor contact them to authorize hospice service. Once they receive that call, they will send out a registered admissions nurse to conduct an assessment of why parents need.
Hopefully, they will be able to schedule an appointment with the registered admissions nurse to coincide with my upcoming trip to Chicago at the end of the week: May 31 through June 5, 2007.
I will keep my fingers crossed, that my parents will both be accepted and that we will soon begin to receive professional help with things we don't know how to handle emotionally.
I will keep you posted on the outcome.









.jpg)
No comments:
Post a Comment